Introduction
Definition of Atrial Fibrillation (AF)
Atrial fibrillation (AF) is a common cardiac arrhythmia characterized by irregular and often rapid heartbeats.
In AF, the heart’s upper chambers (atria) beat chaotically and out of coordination with the lower chambers (ventricles), leading to ineffective blood pumping.
Importance of Understanding AF in Cardiology
AF is a significant health concern due to its association with an increased risk of stroke, heart failure, and other cardiovascular complications.
Understanding AF is crucial for cardiologists and healthcare professionals to effectively diagnose, manage, and prevent associated complications.
Prevalence and Significance of AF Globally and in India
AF is the most common sustained cardiac arrhythmia worldwide, affecting millions of people.
In India, the prevalence of AF is rising due to factors such as the aging population, increasing prevalence of risk factors like hypertension and diabetes, and improved detection methods.
The burden of AF in India poses substantial healthcare challenges and underscores the need for comprehensive management strategies.
Book Your Appointment
Take the first step towards a healthier heart. Book your appointment to consult with Dr. Sachinkumar Patil and embark on your journey to optimal cardiovascular health. Your heart deserves expert care – schedule your appointment today.
Understanding Atrial Fibrillation
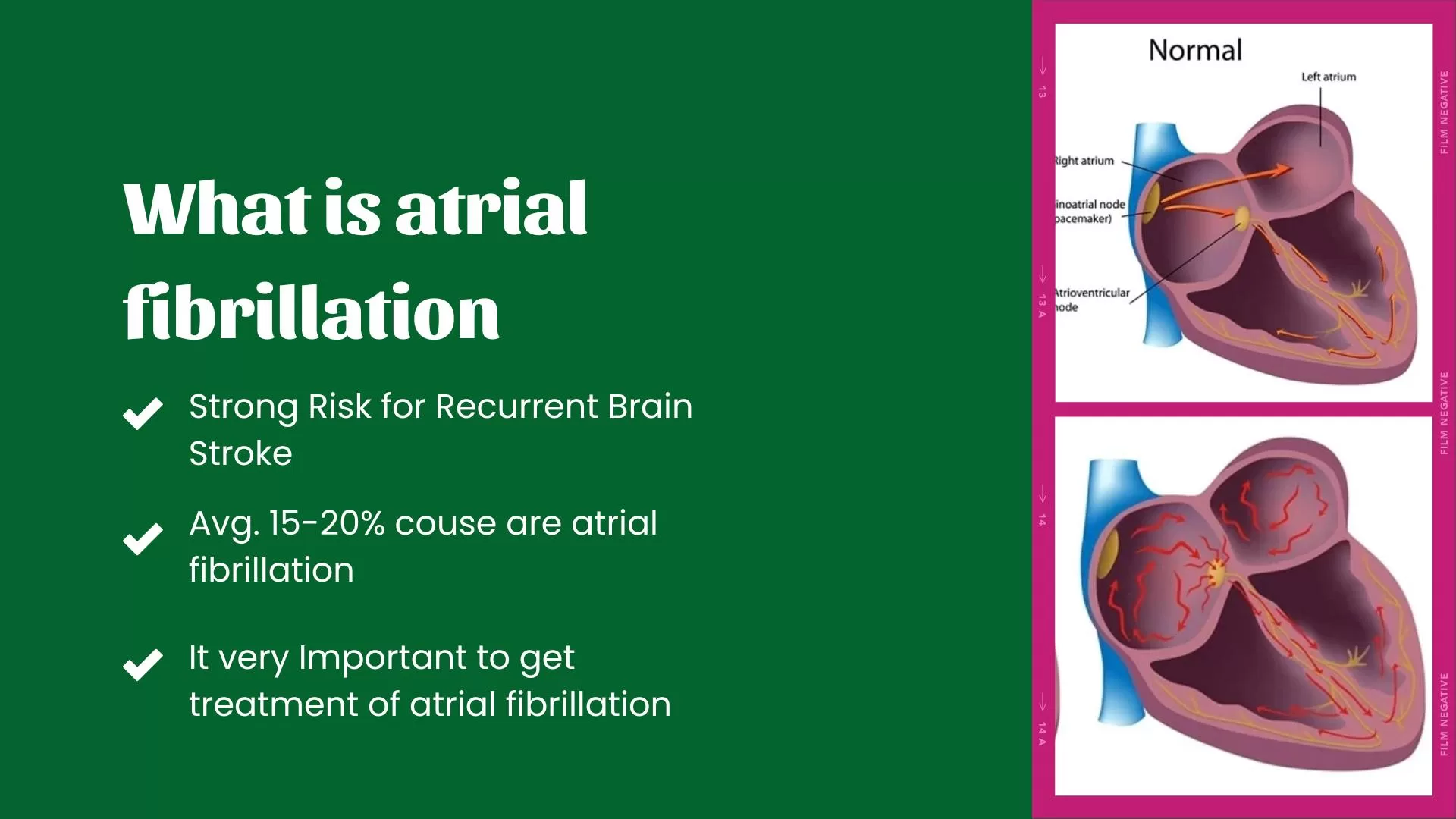
Explanation of the Heart’s Electrical System
The heart’s electrical system coordinates the timing and sequence of heartbeats to ensure efficient blood pumping throughout the body.
It consists of specialized cells that generate electrical impulses, which travel through the heart in a coordinated manner and cause rhythmic contractions.
Mechanism of Atrial Fibrillation
Atrial fibrillation occurs when abnormal electrical signals disrupt the normal rhythm of the heart’s atria.
Instead of the usual coordinated contraction, the atria fibrillate, or quiver, rapidly and irregularly.
This chaotic electrical activity results in an irregular heartbeat and ineffective blood pumping into the ventricles.
Types of AF (Paroxysmal, Persistent, Long-standing Persistent, and Permanent)
Paroxysmal AF:
Paroxysmal AF refers to episodes of irregular heart rhythm that start suddenly and typically stop on their own within 48 hours, although they can persist for up to a week.
These episodes may occur sporadically and may not require long-term treatment.
Persistent AF:
Persistent AF occurs when episodes of irregular heart rhythm last longer than seven days and do not stop spontaneously.
Medical intervention or cardioversion may be required to restore normal sinus rhythm.
Long-standing Persistent AF:
Long-standing persistent AF is characterized by continuous irregular heart rhythms lasting more than one year.
Despite attempts to restore normal rhythm, AF persists without successful treatment.
Permanent AF:
Permanent AF occurs when attempts to restore normal sinus rhythm are unsuccessful or not attempted due to underlying conditions or patient preference.
Patients with permanent AF typically require long-term management to control symptoms and reduce complications.
Understanding the different types of AF helps guide treatment decisions and prognosis for patients with this condition.
Book Your Appointment
Take the first step towards a healthier heart. Book your appointment to consult with Dr. Sachinkumar Patil and embark on your journey to optimal cardiovascular health. Your heart deserves expert care – schedule your appointment today.
Risk Factors for Atrial Fibrillation
A. Age and Gender
Age is a significant risk factor for atrial fibrillation, with the prevalence of AF increasing with advancing age.
AF is more common in older adults, particularly those over 65.
Gender also plays a role, with men generally having a higher risk of developing AF than women, although the gender gap diminishes with advancing age.
B. Hypertension
Hypertension, or high blood pressure, is a leading risk factor for atrial fibrillation.
Elevated blood pressure increases the workload on the heart and can lead to structural changes in the heart’s chambers, increasing the risk of arrhythmias, including AF.
C. Heart Diseases
Various heart diseases increase the risk of atrial fibrillation, including:
1. Coronary Artery Disease (CAD):
Narrowing or blockage of the coronary arteries can decrease blood flow to the heart muscle, increasing the risk of AF.
2. Valve Disorders:
Conditions such as mitral valve prolapse or stenosis can disrupt the normal flow of blood through the heart, predisposing individuals to AF.
D. Obesity and Lifestyle Factors
Obesity is associated with an increased risk of atrial fibrillation, likely due to its association with hypertension, diabetes, and other cardiovascular risk factors.
Lifestyle factors such as smoking and excessive alcohol consumption have been linked to an elevated risk of AF.
Smoking contributes to inflammation and oxidative stress, while excessive alcohol intake can directly affect the heart’s electrical properties and increase the likelihood of arrhythmias.
E. Other Medical Conditions
Thyroid Disorders:
Thyroid dysfunction, particularly hyperthyroidism (overactive thyroid), can predispose individuals to atrial fibrillation by affecting heart rate and rhythm.
Diabetes:
Diabetes mellitus is a significant risk factor for AF, with poorly controlled blood sugar levels contributing to endothelial dysfunction, inflammation, and structural changes in the heart.
Understanding these risk factors helps identify individuals at higher risk of developing atrial fibrillation and implement preventive measures and early interventions to reduce the likelihood of AF and its associated complications.
Book Your Appointment
Take the first step towards a healthier heart. Book your appointment to consult with Dr. Sachinkumar Patil and embark on your journey to optimal cardiovascular health. Your heart deserves expert care – schedule your appointment today.
IV. Signs and Symptoms
A. Palpitations
– Palpitations, or a sensation of rapid, fluttering, or pounding heartbeats, are a common symptom of atrial fibrillation.
– Patients may describe feeling their heart racing or irregularly beating, even at rest.
B. Fatigue
– Fatigue or unusual tiredness is frequently reported by individuals with atrial fibrillation.
– The irregular heartbeat associated with AF can impair the heart’s ability to effectively pump blood, leading to decreased oxygen delivery to the body’s tissues and increased feelings of fatigue.
C. Shortness of Breath
– Shortness of breath, also known as dyspnea, may occur with exertion or even at rest in individuals with atrial fibrillation.
– The irregular heart rhythm and reduced cardiac output can impair lung function, leading to difficulty breathing.
D. Dizziness or Lightheadedness
– Atrial fibrillation can cause feelings of dizziness or lightheadedness, especially when the heart rate becomes excessively rapid or irregular.
– Reduced blood flow to the brain due to ineffective cardiac output can result in these symptoms.
E. Complications of Untreated AF (Stroke, Heart Failure)
– Without appropriate management, atrial fibrillation can lead to serious complications, including stroke and heart failure.
– Blood clots may form in the heart’s chambers due to stagnant blood flow, increasing the risk of stroke if these clots travel to the brain.
– Chronic atrial fibrillation can also weaken the heart muscle over time, leading to heart failure and its associated symptoms, such as fatigue, shortness of breath, and fluid retention.
Recognizing the signs and symptoms of atrial fibrillation is crucial for early diagnosis and intervention to prevent complications and improve patient outcomes.
Valuable insights and guidance on the procedure and its implications for heart health.
For More About Interventional Cardiology
Book Your Appointment
Take the first step towards a healthier heart. Book your appointment to consult with Dr. Sachinkumar Patil and embark on your journey to optimal cardiovascular health. Your heart deserves expert care – schedule your appointment today.