Interventional Cardiologist: Pioneers of Heart Health
In modern medicine, interventional cardiology is a beacon of hope for those grappling with cardiovascular issues. From innovative procedures to advanced diagnostic tests, interventional cardiologists are at the forefront of battling heart disease and enhancing patients’ quality of life. Let’s delve into the world of interventional cardiology, exploring its essence, procedures, and the role of these medical professionals in safeguarding cardiac health.
What is Interventional Cardiology?
Interventional cardiology is a specialized branch of medicine dedicated to managing cardiovascular conditions using minimally invasive techniques. This field focuses on diagnosing and treating many heart diseases, including coronary artery disease, heart valve disorders, and peripheral vascular disease.
Rather than resorting to traditional open-heart surgeries, interventional cardiologists utilize advanced technologies and catheter-based procedures to access the heart and its blood vessels through small incisions. These procedures often involve inserting catheters into arteries or veins and navigating them to the affected area under imaging tools such as fluoroscopy or intravascular ultrasound.
Once the catheter is in place, various interventions can be performed, such as angioplasty to widen narrowed arteries, stent placement to keep streets open, and closure of structural defects in the heart. These minimally invasive techniques offer several advantages over conventional surgery, including reduced recovery times, shorter hospital stays, and lower risks of complications.
Interventional cardiology is crucial in improving patient outcomes and quality of life by providing effective treatment options for cardiovascular conditions while minimizing discomfort and recovery periods. This field continues to evolve with advancements in technology and techniques, allowing interventional cardiologists to address increasingly complex cases with greater precision and efficacy.
History of Interventional Cardiology
Interventional cardiology has come a long way since its inception. Dr. Andreas Gruentzig performed the first coronary angioplasty, a groundbreaking procedure, in 1977. This laid the foundation for a rapidly evolving field offering less invasive options for heart patients.
Interventional Cardiology vs. Cardiothoracic Surgery
Interventional cardiology and cardiothoracic surgery are two distinct specialties within the realm of cardiovascular medicine, each with its own set of approaches and procedures for managing heart conditions.
Interventional cardiology focuses on performing minimally invasive procedures to diagnose and treat cardiovascular diseases. These procedures typically involve accessing the heart and its blood vessels through small incisions in the skin, often using catheters guided by imaging techniques. Common interventions include angioplasty, where a balloon-tipped catheter is used to widen narrowed arteries, and stent placement to keep arteries open. Other procedures may involve repairing structural defects in the heart or removing blockages in blood vessels.
In contrast, cardiothoracic surgery involves open-heart procedures that require accessing the heart and surrounding structures through a larger incision in the chest. Cardiothoracic surgeons are trained to perform complex surgeries such as coronary artery bypass grafting (CABG), where blocked arteries are bypassed using blood vessels from elsewhere in the body, and heart valve repair or replacement procedures. These surgeries often require the use of cardiopulmonary bypass, a machine that temporarily takes over the function of the heart and lungs during the procedure.
While both interventional cardiology and cardiothoracic surgery are effective in treating heart conditions, the choice between them depends on various factors such as the patient’s medical history, the severity and complexity of the condition, and individual preferences. Interventional cardiology may be preferred for less invasive interventions with quicker recovery times, while cardiothoracic surgery may be necessary for more complex cases requiring open-heart procedures. Ultimately, the decision is made collaboratively between the patient, cardiologist, and cardiothoracic surgeon to ensure the best possible outcome for the individual.
Specialization of Interventional Cardiologists
Cardiologists who specialize in interventional procedures concentrate on identifying and addressing different cardiovascular conditions, including peripheral vascular disease, heart valve disorders, and coronary artery disease. These specialists possess the necessary expertise for performing intricate procedures that can help restore blood circulation to the heart and alleviate symptoms like chest pain and shortness of breath.
Diagnostic Tests Ordered by Interventional Cardiologists
Diagnostic testing is critical to interventional cardiology, providing valuable insights into cardiac function and identifying underlying conditions that may require intervention. Interventional cardiologists may order a variety of diagnostic tests to evaluate patients comprehensively. Some of the critical diagnostic modalities used in interventional cardiology include:
Computed Tomography (CT) Angiography:
CT angiography is a non-invasive imaging technique that uses X-rays and computer technology to create detailed images of the coronary arteries and detect any blockages or narrowing. This imaging modality provides high-resolution images of the heart and blood vessels, aiding in diagnosing coronary artery disease and guiding treatment decisions.
Intracardiac Echocardiography (ICE):
ICE is a specialized form of echocardiography that involves inserting a tiny ultrasound probe into the heart via a catheter placed in a blood vessel. This allows for real-time imaging of the heart’s structures and blood flow, providing valuable information about heart function, valve abnormalities, and structural defects.
Cardiac Magnetic Resonance Imaging (MRI):
Cardiac MRI is a non-invasive imaging technique that uses powerful magnets and radio waves to create detailed images of the heart and surrounding structures. This imaging modality can assess cardiac function, myocardial viability, and the presence of scar tissue or abnormalities in the heart muscle.
Chest X-ray:
Chest X-rays are commonly used to evaluate the size, shape, and position of the heart and lungs. While not as detailed as other imaging modalities, chest X-rays can provide valuable information about the presence of heart enlargement, fluid in the lungs (pulmonary edema), or signs of heart failure.
In addition to these imaging tests, interventional cardiologists may perform various other diagnostic procedures, such as cardiac catheterization, stress testing, and blood tests, to assess cardiac biomarkers. These diagnostic tests are crucial in guiding treatment decisions, monitoring disease progression, and optimizing outcomes for patients with cardiovascular conditions. By utilizing a multidisciplinary approach and state-of-the-art diagnostic techniques, interventional cardiologists strive to provide comprehensive, personalized care to individuals with heart disease.
Interventional Cardiac Procedures
Interventions performed by interventional cardiologists cover a range of methods to improve cardiac function and restore normal blood flow to the heart. Angioplasty is commonly used to widen narrowed arteries using a balloon, while stent placement is employed to keep arteries open. Additionally, catheter-based interventions are available for structural heart defects, and thrombectomy is another procedure that can be used to remove blood clots.
Most Common Procedure Performed by Interventional Cardiologists
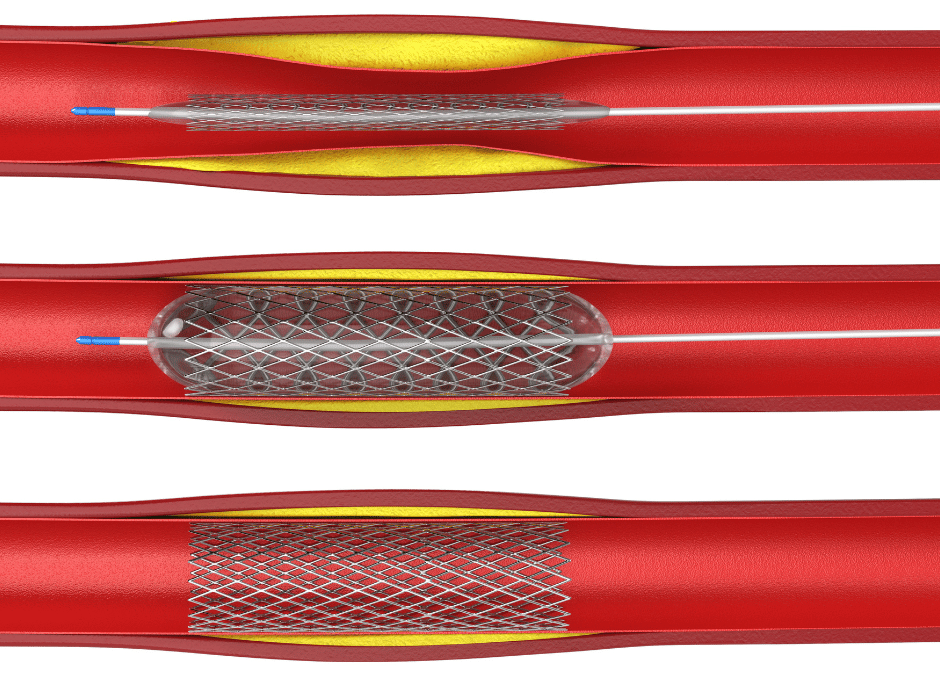
Angioplasty, also known as percutaneous coronary intervention (PCI), is a cornerstone procedure in interventional cardiology. It is frequently employed to treat coronary artery disease (CAD). During angioplasty, a thin, flexible catheter equipped with a deflated balloon is inserted into the narrowed coronary artery. Once in position, the balloon is inflated, compressing the plaque and widening the artery to restore blood flow to the heart muscle.
In many cases, the placement of a stent accompanies angioplasty to help keep the artery open and prevent it from re-narrowing—a process known as restenosis. Stents are small mesh tubes made of metal or fabric that are expanded within the artery using the balloon catheter. Once expanded, the stent remains in place, acting as a scaffold to support the artery and maintain its patency.
Angioplasty and stent placement offer several benefits over traditional open-heart surgery, including shorter recovery times, reduced risk of complications, and improved quality of life for patients. These minimally invasive procedures have revolutionized the treatment of CAD, providing effective solutions for relieving chest pain (angina), preventing heart attacks, and improving overall cardiac function.
As technology and techniques continue to advance in interventional cardiology, angioplasty and stent placement remain integral components of the cardiologist’s armamentarium, offering hope and healing to countless individuals afflicted by coronary artery disease and other cardiovascular conditions.
Diseases and Conditions Treated by Interventional Cardiology
Interventional cardiology is crucial in managing various cardiovascular diseases and conditions, employing innovative techniques to improve patient outcomes and enhance cardiovascular health. Some of the critical diseases and conditions treated by interventional cardiologists include:
Coronary Artery Disease (CAD):
CAD occurs when the blood vessels that supply oxygen-rich blood to the heart become narrowed or blocked due to the buildup of plaque—a condition known as atherosclerosis. Interventional cardiologists perform procedures such as angioplasty and stent placement to restore blood flow to the heart and alleviate symptoms such as chest pain (angina).
Myocardial Infarction (Heart Attack):
A heart attack occurs when blood flow to a part of the heart muscle is blocked, leading to tissue damage or death. Interventional cardiologists play a critical role in managing acute myocardial infarction by performing emergency angioplasty and stent placement to reopen blocked arteries and minimize cardiac damage.
Heart Valve Disorders:
Valve disorders such as aortic stenosis (narrowing of the aortic valve) or mitral regurgitation (leakage of the mitral valve) can impair heart function and lead to symptoms such as shortness of breath and fatigue. Interventional cardiologists may perform transcatheter valve interventions, including valve repair or replacement, using minimally invasive techniques.
Peripheral Arterial Disease (PAD):
PAD involves narrowing or blockage of the arteries outside the heart, typically affecting the arteries in the legs. Interventional cardiologists can perform procedures such as angioplasty, stent placement, or atherectomy to improve blood flow to the legs and alleviate symptoms such as leg pain and cramping.
Congenital Heart Defects:
Some individuals are born with structural abnormalities of the heart, known as congenital heart defects. Interventional cardiologists collaborate with pediatric cardiologists and cardiac surgeons to diagnose and treat these conditions, often performing catheter-based interventions to repair defects without the need for open-heart surgery.
By leveraging cutting-edge technologies and techniques, interventional cardiologists strive to alleviate symptoms, prevent complications, and improve overall cardiovascular health for patients with these and other cardiac conditions. Their multidisciplinary approach, coupled with a commitment to innovation and excellence, ensures that individuals receive personalized, comprehensive care tailored to their unique needs and circumstances.
Training for Interventional Cardiology
Becoming an interventional cardiologist requires rigorous training and specialization. Aspiring cardiologists who have completed medical school and internal medicine residency must undergo fellowship training in interventional cardiology. This training program focuses primarily on advanced cardiac catheterization techniques, procedural skills, and patient care.
Expectations at an Interventional Cardiology Appointment
Patients can anticipate comprehensive evaluation during an interventional cardiology appointment, including a thorough medical history review, physical examination, and diagnostic testing as warranted. Depending on the findings, the interventional cardiologist will discuss treatment options, including potential procedures, and formulate a personalized management plan tailored to the patient’s needs.
Contact Us
Ready to prioritize your heart health? Contact us today through our contact page and let’s discuss your personalized care plan.
What are the risks associated with interventional cardiology procedures?
Interventional cardiology procedures carry inherent risks, including bleeding, infection, allergic reactions to contrast dye, and complications such as blood vessel injury or clot formation. However, the benefits often outweigh the risks, particularly in patients with significant cardiovascular disease.
Is interventional cardiology suitable for all heart conditions?
While interventional cardiology offers effective treatment options for many heart conditions, not all patients may be suitable candidates for these procedures. Factors such as the severity of the disease, overall health status, and individual patient preferences are considered when determining the appropriateness of interventional interventions.
How long does recovery take after an interventional cardiology procedure?
The recovery duration depends on the procedure type and various factors specific to each patient. Typically, those who undergo minimally invasive treatments such as angioplasty and stenting experience shorter recovery periods than those who have open-heart surgeries. With the assistance of their healthcare providers, patients may generally resume their regular activities within a few days to weeks.
Are there alternative treatments to interventional cardiology procedures?
In some cases, alternative treatments such as medication therapy, lifestyle modifications, and cardiac rehabilitation may be viable options for managing cardiovascular conditions. Interventional cardiology procedures are typically recommended when conservative measures fail to control symptoms or mitigate disease progression adequately.
In conclusion, interventional cardiology epitomizes the marriage of innovation and precision in cardiovascular care. With a steadfast commitment to excellence and a patient-centered approach, interventional cardiologists continue revolutionizing the treatment landscape, offering hope and healing to heart disease patients. If you’re seeking comprehensive cardiac care, entrust your heart to the skilled hands of an interventional cardiologist and embark on a journey toward optimal heart health.